Healthcare Credentialing: A Comprehensive Overview
It is hard to stay on top of ever-changing processes. As Community Healthcare Center (CHC) and Federally Qualified Healthcare Center (FQHC) leaders, you simply don’t have time to spend hours sifting through files and watching webinars to get the information you need for successful credentialing and enrollment.
Our team of experts makes this education a top priority and creates a comprehensive overview of your healthcare credentialing process for you.
What is credentialing?
Credentialing is the process of verifying the qualifications of healthcare providers.
This important safety check is the first step before a provider can work in your healthcare organization.
It is an essential part of ensuring the safety and quality of patient care. Credentialing typically includes verifying a healthcare provider’s education, training, and experience, as well as their criminal background and professional history through a process called Primary Source Verification (PSV), where the organization doing the credentialing reaches out to the source to verify that the information is accurate as represented by the applicant.
What is credentialing and provider enrollment?
Credentialing and provider enrollment are two related processes that are often used interchangeably. However, there is a difference between the two. Credentialing is the process of verifying a healthcare provider is who they say they are, while provider enrollment is the process of adding a healthcare provider to a health plan's network. Our experts highly recommend
integrating the two processes for maximum efficiency and ROI.
Alternative terms for credentialing:
Professional credentialing, provider credentialing, and PSV.
Alternative terms for enrollment:
Financial credentialing and payor enrollment.
What are the stages of credentialing?
The stages of credentialing are:
- Application: The healthcare provider submits an application to the credentialing organization including
- Contact information
- Current CV
- Education and training history
- Licensing and certificates
- Medical group and hospital affiliations
- Board certifications, sanctions, or malpractice history
- Proof of liability insurance
- Peer references
- Verification: The credentialing organization checks that all the above information is correct and up to date.
- Approval: The credentialing organization approves the healthcare providers’ application and issues a credential. The credentialing process can take as little as 30 days or as much as 6+ to complete.
- Renewal: The healthcare provider must renew their credential regularly, typically every one to two years.
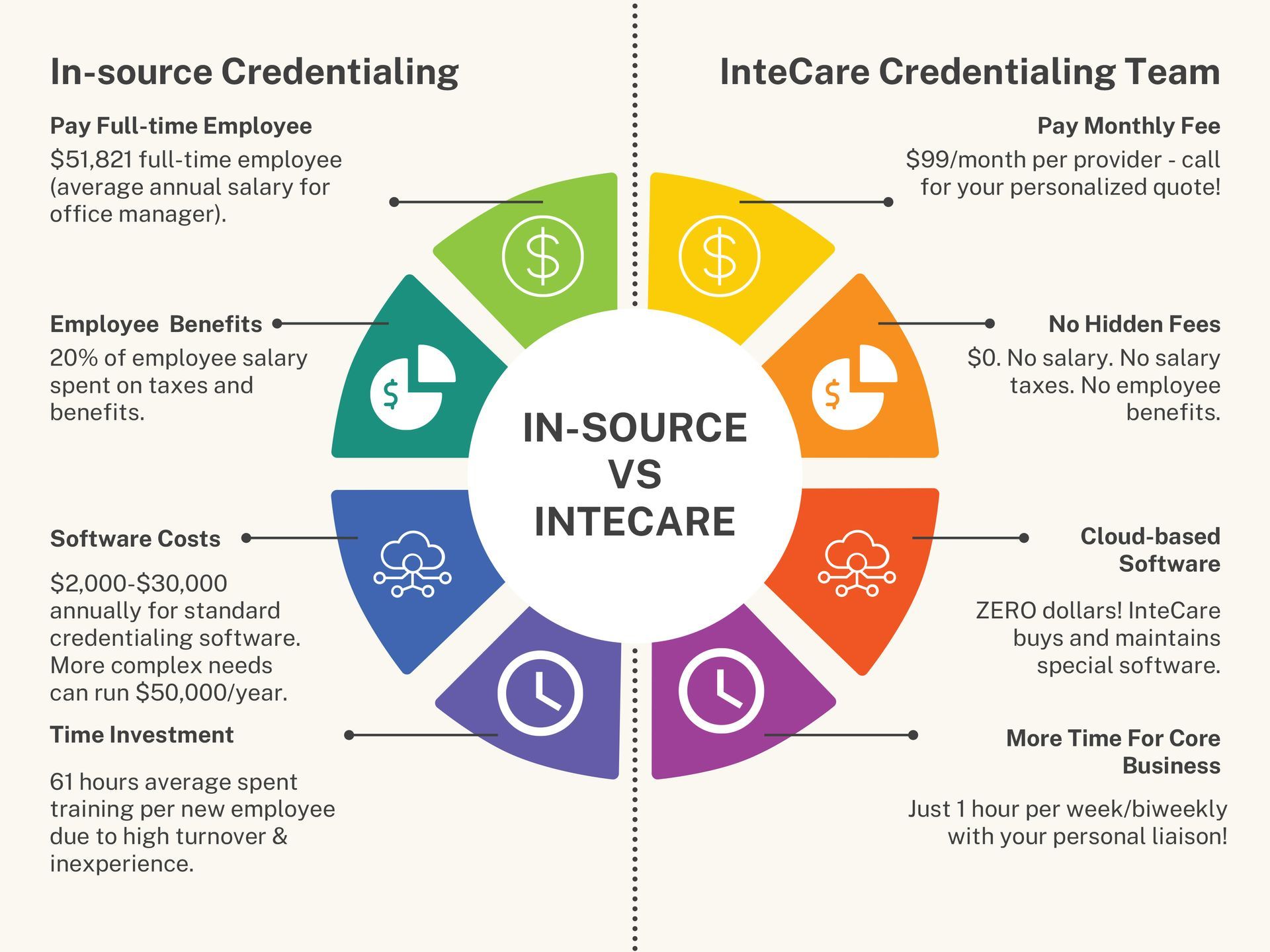
Who does credentialing for new hires?
The responsibility for credentialing new hires typically falls to the HR, billing/claims, or Cred/Enroll department. However, in some cases, the
credentialing process may be outsourced to a third-party credentialing organization, like InteCare.
What are the challenges to successful credentialing?
You’ll face countless obstacles to credentialing and enrolling providers. Your staff must stay on top of ever-changing rules and regulations or risk providers falling out of participating status.
- Time back and forth: The credentialing process can be lengthy and complex, requiring multiple rounds of communication between the healthcare center and the provider. This can eat up valuable time and resources, especially for small healthcare centers with limited staff.
- Specialized knowledge: The credentialing process requires specialized knowledge of healthcare regulations and standards. This can be difficult for healthcare centers to find, especially if they are located in rural areas or have limited resources.
- Wearing many hats: Healthcare center staff often wear many hats, which can make it difficult to focus on the credentialing process. This can lead to errors and delays, which can further complicate the process.
Why is credentialing important in healthcare?
Credentialing is important in healthcare because it helps to ensure the safety and quality of patient care. By verifying the qualifications of healthcare providers, credentialing protects patients from harm and ensures that they receive the highest quality of care possible.
Credentialing also has many benefits for your revenue cycle and internal operations.
- Revenue cycle: Credentialing can help to improve the revenue cycle by reducing the number of denials and appeals. When healthcare providers are properly credentialed, payers are more likely to approve claims. This can lead to faster payments and reduced costs for healthcare organizations.
- Efficiency: Credentialing can also help to improve efficiency by streamlining the process of on-boarding new healthcare providers. When credentialing is done efficiently, healthcare organizations can get new providers up and running faster. This can help to reduce wait times for patients and improve access to care.
- Time: Credentialing can also save time by systematizing the process of verifying healthcare provider qualifications. When credentialing is streamlined, healthcare organizations spend less time on administrative tasks and more time on patient care.
Interested in learning more about outsourcing healthcare credentialing?
Read this blog!

Phone: (317) 237-5770
Fax: (317) 237-5777
Address: 9425 Delegates Row Indianapolis, IN 46240
Phone: (317) 237-5770
Fax: (317) 237-5777
Address: 9425 Delegates Row, Indianapolis, IN 46240