7 Must-Ask Questions For Credentialing & Enrollment Process
7 Must-Ask Questions For Credentialing & Enrollment Process
Healthcare credentialing is the process where medical organizations verify the credentials of healthcare providers to ensure they meet all requirements, including licensing, certifications, and skills to provide safe quality patient care.
It is a long, tedious process often involving time spent researching and staying on top of ever-changing rules and regulations. This is why many FQHC and CHC leaders outsource credentialing and enrollment services to experts who have extensive experience with these complex processes.
Our team of credentialing experts has compiled a list of our most frequently asked questions by FQHC and CHC leaders looking to outsource this hefty administrative burden.
Check out our short and sweet list of FAQs:
#1 How long does it take to get a provider enrolled with payors?
90-120 days, varies, based on how quickly the provider turns over information, when the application is submitted, and the payor. Get PSV done at the same time and maximize efficiency!
#2 Do you provide re-credentialing services?
YES! Never worry about keeping track of which provider is up for re-credentialing. We make sure credentialing is done right and on time.
#3 Do you gather all provider information or do we have to?
We are happy to take on the burden of gathering information directly from the provider so you get more time back.
#4 When do you like to start the process for a new provider?
When you know you want to hire a provider—way before they come on board! Simply give us their personal email for a seamless onboarding process.
#5 How do you determine rates?
As a non-profit, we are committed to keeping our fees low. We understand there is turnover in the FQHC world so we offer monthly pricing based on the actual number of providers on your staff.
For example, if you have 49 providers in January and 50 in February, you’re only billed for the 49 providers one month and 50 the next. .
#6 How long is organizational onboarding?
Depending on the size, it takes 60-90 days until fully onboarded, so that we have everything accurate for payors and ensure the success of your revenue cycle.
#7 Which states can you provide credentialing services in?
We service all 50 states. Our team of experts will learn your specific state requirements and stay on top of the ever-changing rules for you.

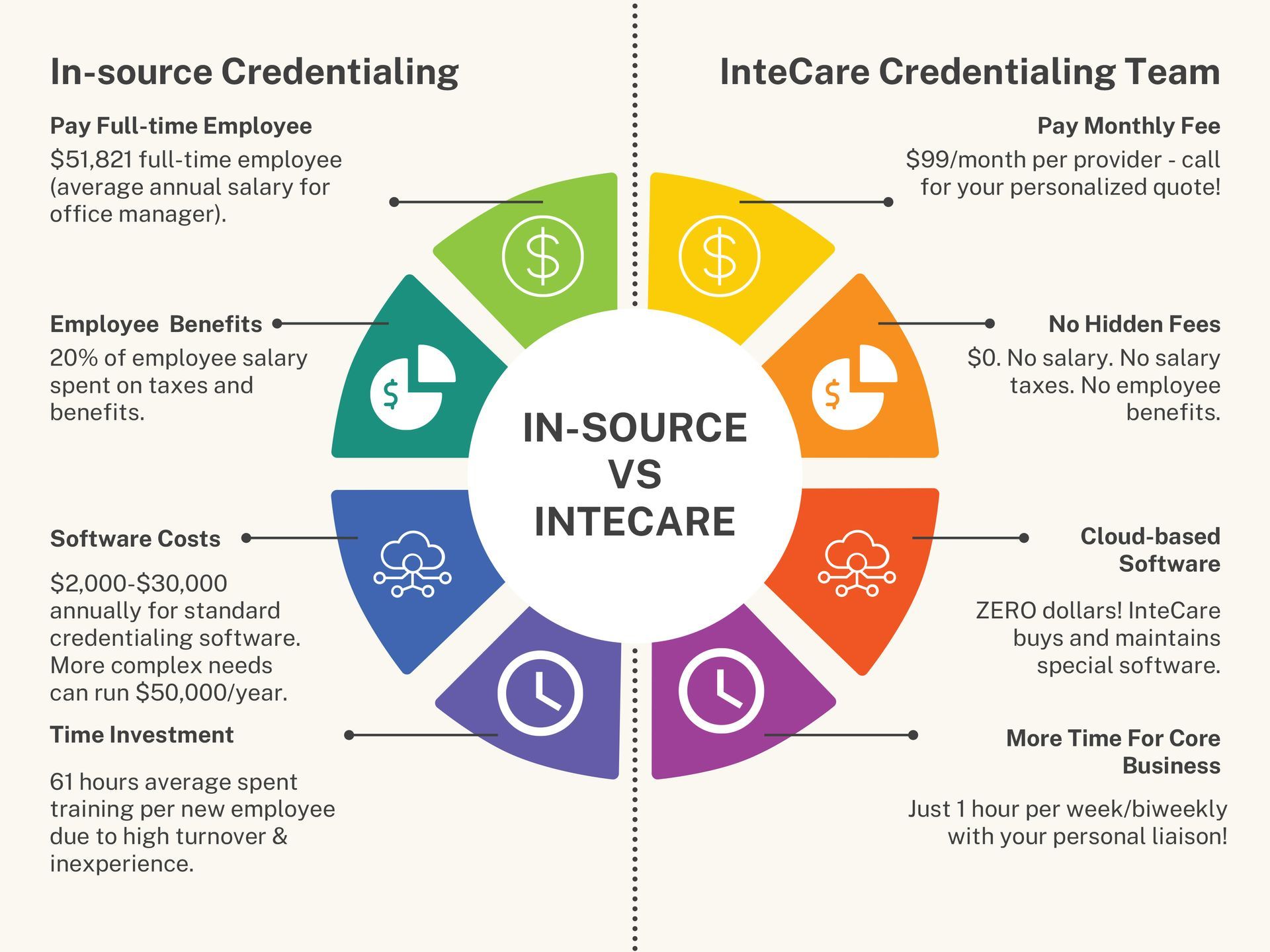
There is no room for course correction when it comes to your operational budget. Wasted time researching leads to higher administrative costs for you.
FQHC and CHC already operate on tight budgets and limited resources, and simply cannot afford missed deadlines, errors, and loss of revenue.
Are you using credentialing experts and the best available tools for this critical process?
InteCare curated an expert team to help you streamline these complex internal processes and maximize your revenue cycle.
- InteCare has served over 3,000 providers.
- All 50 states are serviced.
- 100% of health plans serviced.
You need someone in your corner who understands the unique challenges of credentialing and enrollment.
Remember it’s no longer just about your organization...it’s also about your community.
Are you ready to confidently run your healthcare center, maximize revenue and improve patient and provider satisfaction? All you have to do is
schedule a consultation to get started.
✔️ Initial enrollment with all payors, Medicaid and Medicaid Managed Care Organizations, Medicare and other Medicare Insurance, and all commercial insurers
✔️ Maintain credentialing requirements for each licensed provider throughout the year, including CAQH
✔️ Re-credentialing


Phone: (317) 237-5770
Fax: (317) 237-5777
Address: 9425 Delegates Row Indianapolis, IN 46240
Phone: (317) 237-5770
Fax: (317) 237-5777
Address: 9425 Delegates Row, Indianapolis, IN 46240